Most drug advertisements today include a lot of superficial information touting the benefits of medications, including statistics that can make treatments look fantastic and benign. While the statistics these drug makers cite may be accurate, they’re almost always only telling part of the story.
One of the numbers used in assessing the effectiveness of a drug is the “number needed to treat,” or NNT. As a consumer, knowing the NNT can help you make important decisions about whether or not to take a medication. Yet rarely – if ever – is the NNT included in drug ads.
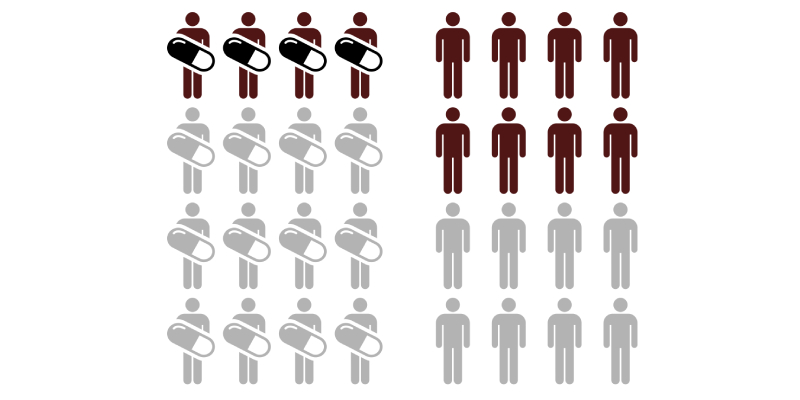
So what is the number needed to treat? It’s the number of patients that would need to be treated in order to achieve the desirable effect or outcome in one patient. For instance, suppose you have a drug that’s intended to prevent stroke. You conduct studies and determine the number needed to treat is 10. What does that mean? It means you would have to treat 10 people with that drug in order to prevent a stroke in one person.
The number needed to treat is a simple way to estimate the potential benefit to be expected from a drug or course of treatment, and it can be an especially helpful marker with respect to comparing one treatment or drug to another.
As noted, the number needed to treat is very rarely included in drug advertising, especially if that number. After all, if the NNT for a new cholesterol drug is 80, that means essentially you’d have a one in 80 chance of having a successful outcome as a result of the medication. Depending on the potential side effects caused by the drug and other factors, you may decide that the benefits and risks just don’t add up.
The NNT can also play an important role in determining negligence of a drug manufacturer whose drug caused significant injury or death.